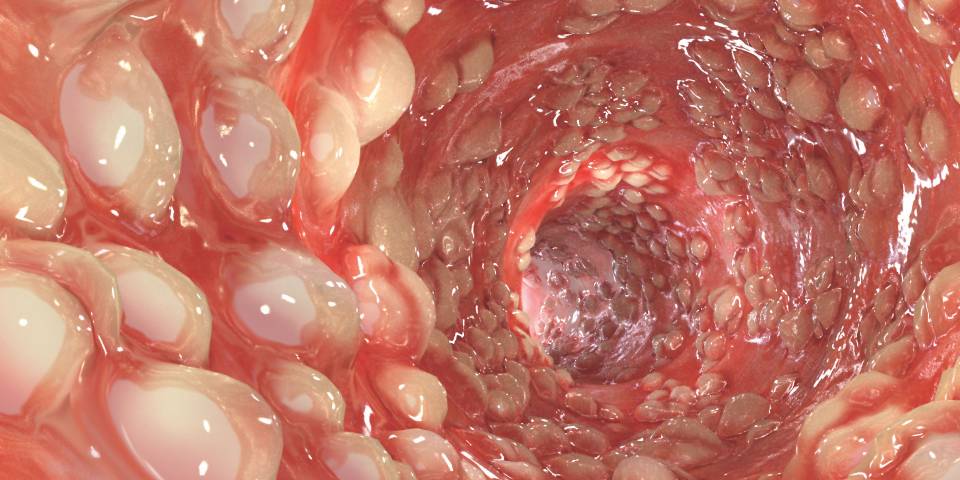
Our digestive system plays a critical part in maintaining overall health, and when something goes wrong, it’s important to act quickly. In India, gastrointestinal( GI) conditions are more common than many realize, affecting 7 out of every 10 people at some point. Recognizing early warning signs can result in significant differences in receiving timely and effective treatment. Consulting an expert like Dr. N Subrahmaneswara Babu, widely regarded as the best gastroenterologist in Hyderabad, ensures you get the best possible care for your digestive health.
What Is a Gastroenterologist?
A gastroenterologist is a doctor who specializes in diagnosing and treating conditions related to the digestive system. This includes your esophagus, stomach, intestines, liver, gallbladder, pancreas, and rectum. These specialists are trained to treat conditions like acid reflux( GERD), gallstones, irritable bowel syndrome( IBS), Crohn’s complaints, and many others.
What Does a Gastroenterologist Do?
A gastroenterologist provides care for patients witnessing digestive troubles. They achieve tests like endoscopies, colonoscopies, and biopsies to check for effects such as ulcers, polyps, or inflammation. They can also suggest lifestyle changes, prescribe drugs, or recommend surgery for more serious conditions.
Now, let’s take a look at,
10 Signs You Need to See a Gastroenterologist:
- Persistent Abdominal Pain: If you have been experiencing constant or recurring pain in your stomach, it might be a sign of an underlying digestive problem. Conditions like ulcers, gallstones, or IBS can affect abdominal pain. However, it’s time to seek expert guidance from the Digestive health specialist in Hyderabad, similar to Dr. N Subrahmaneswara Babu if the pain lasts for days and may worsen.
- Frequent Heartburn or Acid Reflux: Occasional heartburn is common, but if you are feeling that burning sensation in your chest constantly, it could be GERD( Gastroesophageal Reflux Disease). Left untreated, GERD can cause damage to the esophagus. A gastroenterologist can help diagnose and treat this condition.
- Unexplained Weight Loss: Losing weight without any changes in your diet or physical activity can be a red flag. Unintentional weight loss could be linked to serious conditions like Crohn’s disease, celiac disease, or even cancer. Consulting a specialist like Dr. N Subrahmaneswara Babu can assist in identifying the cause.
- Difficulty Swallowing: If you’re having trouble swallowing food or liquids (known as dysphagia), it may be a sign of an issue in your esophagus. Problems like achalasia or esophageal strictures could be the reason behind it, and timely treatment is essential.
- Persistent Diarrhea or Constipation: Everyone experiences digestive problems from time to time, but if you are having persistent diarrhea or constipation, it may point to conditions like IBS, colitis, or colon cancer. These symptoms should never be ignored if they last for more than a few weeks.
- Blood in Your Stool: Seeing blood in your coprolite, whether it’s bright red or darkish, can be alarming. This could be a signal of hemorrhoids, ulcers, or colon cancer. A gastroenterologist will assist to determine the cause and give the right treatment.
- Bloating and Gas: Frequent bloating, gas, or a feeling of fullness can indicate conditions like lactose intolerance, IBS, or small intestinal bacterial overgrowth( SIBO). These symptoms may look minor but can significantly affect your quality of life if left untreated.
- Unexplained Fatigue: Feeling constantly tired or weak, even after a full night’s sleep, could be a signal of malabsorption. Conditions like celiac disease or chronic liver disease can affect how your body absorbs nutrients, leading to fatigue.
- Jaundice (Yellowing of the Skin or Eyes): If you notice yellowing of your skin or eyes, it could be a sign of liver disease or bile duct problems. These conditions require immediate medical attention, and a gastroenterologist like Dr. N. Subrahmaneswara Babu can help diagnose and treat them.
- Change in Bowel Habits: Any significant change in your bowel habits, whether it’s in the frequency, consistency, or color of your coprolite, should be watched. These changes can occasionally indicate conditions like IBD( Inflammatory Bowel complaint), colon polyps, or cancer.
When Should You See a Gastroenterologist?
If you’re experiencing any of the above symptoms, it’s essential to consult a gastroenterologist to get a proper diagnosis and treatment plan. Dr. N. Subrahmaneswara Babu, one of the best GI specialists in Hyderabad, has years of experience treating a wide range of gastrointestinal diseases. Early detection and treatment can prevent complications and enhance your quality of life.
Taking care of your digestive health is important, and knowing when to seek help can make all the difference. If you are looking for expert guidance and treatment from a leading gastroenterologist in Hyderabad. Dr. N. Subrahmaneswara Babu is here to support you. Book an appointment today to ensure you receive the best care for your digestive health.